August 8, 2013 — This article by Lawrence F Muscarella, PhD, provides insight into whether a soiled flexible endoscope’s terminal reprocessing can be delayed for several hours after its clinical use.
Guidelines are reviewed and recommendations are provided.
A protocol for “prepping” the endoscope prior to its delayed reprocessing is provided in a related article by Dr. Muscarella, “Protocol for “Prepping” a GI Endoscope Prior to its Delayed Reprocessing.”
Introduction
The word is used ubiquitously in the lexicon of instrument reprocessing. Namely, guidelines that provide advice for the prevention of disease transmission during gastrointestinal (GI) endoscopy routinely urge staff to reprocess the GI endoscope “immediately” after the procedure.(1-4)
Although this instruction is certain, adherence to it is not foregone.
The more complete article (in PDF format) entitled “The delayed reprocessing of gastrointestinal endoscopes” on which this article is based may be downloaded by clicking here.
Briefly, endoscope reprocessing may be divided into two sequential phases, based on the location within the medical facility where each phase is performed:
1. pre-processing of the endoscope—or phase 1—which is an initial set of reprocessing steps that is performed in the procedure room upon removal of the endoscope from the patient’s GI tract; and
2. terminal reprocessing of the endoscope—or phase 2—which features a more comprehensive set of subsequent reprocessing steps, including leak testing, that is performed once the endoscope is transported to the reprocessing area.(5,6)
When performed properly, in timely sequence, and as recommended by its manufacturer, these two phases render the flexible endoscope safe for reuse, without risk of the endoscope transmitting diseases.(2) [Note: Pre-processing may also be referred to as pre-cleaning or bedside cleaning.(5)]
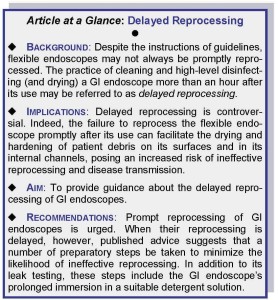
Despite the instructions of guidelines, flexible endoscopes may not always be promptly reprocessed, however. The practice of cleaning and high-level disinfecting (and drying) a GI endoscope more than an hour after its use may be referred to as “delayed reprocessing.”
Two related articles by Dr. Muscarella:
Prompt reprocessing
Box A (embedded, below) provides the recommendation published by several professional organizations and manufacturers to reprocess the GI endoscope immediately after the procedure, the purpose of which is to minimize the likelihood of potentially infectious patient fluids, secretions, and debris drying and hardening on the GI endoscope’s external surfaces and internal channels.(1-4)

Once encrusted, these patient materials can become formidable to remove and may remain on the GI endoscope despite its cleaning, posing an increased risk of ineffective reprocessing, as well as of the GI endoscope’s improper functioning.(6)
While the guidelines of other organizations may use a different adverb such as “promptly,”(7) the importance of reprocessing’s timeliness is no less evident or emphasized.
Indeed, delayed reprocessing is controversial, because the failure to reprocess the flexible endoscope promptly after its use can facilitate the drying and hardening of patient debris on its surfaces and in its internal channels, posing an increased risk of ineffective reprocessing and disease transmission.
The authors of a recently published scientific study concluded that a delay of the GI endoscope’s washing after its use may have resulted in the instrument’s drying, possibly explaining transmission of Klebsiella pneumoniae carbapenemase-producing bacteria.
Delayed reprocessing
No matter the adverb used to describe the imperative, reprocessing the flexible endoscope after the procedure, without delay, is integral to patient safety and the prevention of healthcare-associated infections (HAIs).(1-7)
Nevertheless, on occasion, the GI endoscope’s pre-processing (phase 1) or terminal reprocessing (phase 2) may be delayed for more than an hour* after the procedure.
This scenario—which may be described as “delayed reprocessing”— is not without controversy, because, as displayed in Box A (above), any delay in the endoscope’s cleaning and high-level disinfection is inconsistent with the instructions of published reprocessing guidelines.(1-7)
Yet, even a well-managed out-patient endoscopy center may encounter a “reprocessing bottleneck” that results in the GI endoscope’s delayed reprocessing.
[Note: “One hour” is usually the time specified to define “delayed reprocessing,” because the endoscope manufacturer’s reprocessing instructions have typically been validated for effectiveness up to, but generally not longer than, one hour after the GI endoscopic procedure.(5)]
Quality and Safety Services and Case Reviews for Hospitals, Manufacturers, Patients: Click here to read about Dr. Muscarella’s quality and safety services committed to reducing the risk of healthcare-associated infections, including CRE outbreaks linked to contaminated endoscopes and other reusable medical equipment.
“24 hours a day, 7 days a week”
Endoscope reprocessing is as important to the prevention of HAIs as it can be challenging to manage and delegate.
Although it is ideal for a medical facility to have available at all times, “24 hours a day, 7 days a week,” trained (if not also certified) staff to ensure the timely (i.e., within one hour of its use) reprocessing of every GI endoscope model in inventory—indeed, it would seem to be necessary of any hospital that performs emergency GI endoscopic procedures during “off hours” or late in the night—the expense of having such trained staff always available can be financially prohibitive for some medical facilities.
As a consequence, the reprocessing of GI endoscopes may be delayed. Even a well-managed outpatient GI endoscopy center that performs procedures only during normal working hours is likely to encounter an occasional “reprocessing bottleneck” that, too, may delay the timely reprocessing of GI endoscopes.
No matter whether due to the unavailability of trained reprocessing staff or to a reprocessing bottleneck, delaying a GI endoscope’s reprocessing seems counter-intuitive and inapt, and it can pose an increased risk of disease transmission.
An alternative
An alternative to delaying the reprocessing of a GI endoscope until trained staff are available, or a bottleneck is resolved (possibly as many as several hours later), may be to assign untrained members of the staff — whose knowledge and understanding of the GI’s endoscope’s design and demanding reprocessing requirements may be admittedly limited or poor — the responsibility of reprocessing the GI endoscope promptly after its use.(6)
But, like delayed reprocessing, this alternative, too, can have potentially adverse infection-control consequences, having been reportedly associated with deviations in reprocessing practices.(6)
Indeed, the ineffective reprocessing of flexible endoscopes, including (but not limited to) their improper “leak testing,” has been linked to patient morbidity and mortality.(3,8,9)
“To reprocess or not reprocess?”
The delayed reprocessing of a GI endoscope is as anomalous for its contravention of Box A’s instruction (see above) to reprocess the GI endoscope immediately after its use as it is inevitable.
At some time, virtually every medical facility performing GI endoscopy will be faced with the dilemma “to reprocess or not to reprocess”—namely, to have untrained staff members reprocess the GI endoscope promptly after its use or instead to delay the GI endoscope’s reprocessing until trained reprocessing staff are available.
Aim
Often, the outcome of this quandary is the latter, and the endoscope’s reprocessing is delayed. Therefore, a number of infection-control guidelines, published papers, and the reprocessing instructions of different manufacturers of GI endoscopes were reviewed for guidance about delayed reprocessing.
This article also identifies whether a set of instructions has been published for pre-treating the GI endoscope prior to a delay in its reprocessing, to reduce the likelihood of patient materials drying and hardening on the GI endoscope’s surfaces.
The Center for Public Integrity: Instruments in hospitals “sometimes sit around for hours, or days, before they are cleaned, which allows blood and tissue to dry and harden.” (10,11)
Findings
Some published advice about the delayed reprocessing of GI endoscopes was identified during this review, and it is summarized in Box B, which is embedded below.(1,4-6,12-14)
This review also identified a set of instructions published by one manufacturer of GI endoscopes (Olympus America) that seemingly condones delayed reprocessing, albeit conditionally and provided, for example, that it is not routinely practiced (delayed reprocessing’s deviation from the recommendation to reprocess the GI endoscope promptly after its use notwithstanding).(4-6) [This review did not identify another manufacturer of GI endoscopes that discusses delayed reprocessing.(4-6)]
This review also identified several competency checklists that may help readers better understand the necessary steps both to pre-process and terminally reprocess GI endoscopes.(15-17)

Discussion
Detailed in Box A (above), the “standard” practice of endoscope reprocessing is defined by the GI endoscope’s immediate pre-processing in the procedure room (phase 1) followed by the GI endoscope’s transportation to—and its prompt leak testing, manual cleaning, and terminal high-level disinfection (or sterilization) in—the dedicated reprocessing room or area (phase 2).(5)
After the completion of these two phases, the endoscope may be safely reused or stored in accordance with its manufacturer’s instructions.
Some circumstances may occasionally arise, however, that interfere with the GI endoscope’s prompt reprocessing (the instructions in Box A, above, notwithstanding). From these circumstances arises the term delayed reprocessing, which is defined as terminally reprocessing the GI endoscope more than an hour after its clinical use.
Warranting circumspection, delayed reprocessing may pose an increased risk of HAIs, due to the potential for infectious patient debris to dry on the GI endoscope’s surfaces during this hiatus.
Once hardened and encrusted, this debris can shield and protect underlying infectious agents, preventing their removal and destruction during the GI endoscope’s terminal reprocessing.
“Prepping” the GI endoscope
Even though GI endoscopes are labeled to be reprocessed promptly or immediately after their use (see: Box A, embedded above),(4,16-18) some published guidance discusses their delayed reprocessing (see: Box B, embedded above), and one manufacturer condones it—albeit conditionally, provisionally, and provided the GI endoscope is pre-treated, or “prepped” prior to its terminal reprocessing more than an hour later.(4-6,13)
Briefly, this manufacturer’s procedure for “prepping” the GI endoscope features, in sequence, its leak testing; the flushing of its channels with a detergent solution; followed by its prolonged immersion in the detergent solution (for up to, but not longer than, 10 hours).(6)
Once trained reprocessing staff become available (or a reprocessing bottleneck is resolved), the GI endoscope is then cleaned and terminally high-level disinfected, either manually or using an automated endoscope reprocessor, followed by its reuse or storage.
[Note: Some manufacturers may similarly recommend that the GI endoscope be immersed in a detergent solution during its transportation from the procedure room to the reprocessing area for “standard” terminal reprocessing. Refer to the GI endoscope’s instructions.]
Moreover, as this manufacturer has published, a number of important caveats are associated with “prepping” the GI endoscope for its delayed reprocessing (as many as 10 hours later).
Namely, prolonged immersion:
- should be performed “only when necessary” (according to this manufacturer, unnecessary immersions should be “avoided”);(4,5)
- may damage the GI endoscope if performed routinely or consecutively;(4-6,13) and
- is an additional reprocessing step that is not a replacement for the GI endoscope’s manual cleaning or terminal
reprocessing.(5)
Limiting this “prepping” procedure’s uses, this manufacturer counsels that it only be performed, in addition to when the GI endoscope was not promptly reprocessed after its use, when the GI endoscope’s surfaces are suspected of being contaminated with hardened patient debris and/or when the GI endoscope was used during a procedure with excessive bleeding.(4-6,13)
Based, in part, on this manufacturer’s published procedure, a more detailed protocol that may be suitable for the delayed reprocessing of a GI endoscope (or of another type of flexible endoscope or comparable reusable medical instrument) was developed and, for the reader’s convenience, is provided in another article, which can be read by clicking here. (Several caveats and restrictions that apply to this protocol are also discussed in this other article.)
For clarification, this article discusses, but does not endorse, the delayed reprocessing of GI endoscopes and other types of reusable medical instruments.
Readers are encouraged to discuss with the manufacturer(s) of their GI endoscopes the appropriateness of delayed reprocessing and of the protocol detailed in another of Dr. Muscarella’s articles (click here to read it), which includes the GI endoscope’s prolonged immersion in a detergent solution.
Indeed, failure to clean and high-level disinfect (and dry) the GI endoscope promptly after its clinical use may result in the drying of patient materials, ineffective reprocessing and damage to the GI endoscope voiding its warranty.(1-7,10-14)
Note: The prolonged immersion of a GI endoscope is an additional reprocessing step—it is not a replacement for manual cleaning or terminal reprocessing.
Summary and recommendations
Reprocessing the GI endoscope promptly after its use is urged (see: Box A, embedded above). Otherwise, the risk of its ineffective reprocessing (and of damage to its materials) may increase.
Nevertheless, if the GI endoscope’s reprocessing is delayed, whether due to the limited availability of trained staff or to a reprocessing bottleneck, or if the GI endoscope either was used during a procedure with excessive bleeding or is suspected of being contaminated with hardened patient debris, users of GI endoscopes manufactured by one company (Olympus America) may “prep” the GI endoscope prior to its terminal reprocessing more than an hour later—provided, however, that several caveats are understood and criteria are satisfied (see: Box B, embedded above).(4-6,13)
This manufacturer’s procedure for delayed reprocessing is included in the reprocessing manuals of most of its GI endoscopes, and its review by the reader is recommended.(5)
Another article, which can be read by clicking here, provides a detailed step-by-step protocol that may be (but is not necessarily) suitable when a GI endoscope’s reprocessing is delayed.
Prior to performing this protocol, the manufacturer’s procedure,(4) or another comparable one, however, it is recommended that the medical facility be circumspect and first contact the instrument’s manufacturer(s) to discuss delayed reprocessing and whether the step-by-step procedure provided in this other article, or a comparable one that includes the GI endoscope’s prolonged immersion in a detergent solution, is suitable or might instead damage the instrument and void its warranty.
Review of any of several published competency checklists for reprocessing GI endoscopes is also recommended to enhance the quality of infection control.(15-17)
The use of water, without detergent, to “pre-clean” the GI endoscope in the procedure room is discussed in a third related article by Dr. Muscarella, which can be read by clicking here.
In closing, prompt reprocessing of GI endoscopes is recommended. When their reprocessing is delayed, however, a number of preparatory steps may possibly be performed with caution to minimize the likelihood of ineffective reprocessing. In addition to its leak testing, these steps include the GI endoscope’s prolonged immersion in a suitable, compatible detergent solution.
This article’s references are available by clicking here.
Article by: Lawrence F Muscarella, PhD, posted on 3-7-2013; updated: 10/1/2015, Rev. A.