This article by Lawrence F Muscarella, PhD, discusses whether 2% glutaraldehyde formulations and peracetic acid solutions, either of which may be used to achieve high-level disinfection, might cause damage of immersed flexible endoscopes. This article is based on a more comprehensive article that may be read by clicking here.
This is the first of two articles that discuss endoscope damage potentially caused by disinfectants and sterilants. Click here to read the second article in this series, along with a set of important recommendations.
The two articles in this series were originally written in 2009.
SUMMARY OF ARTICLE
An evaluation of the Steris Reliance EPS was published in 2007. Authored by the ECRI Institute, this evaluation includes Steris’s claim that peracetic acid—used by the Reliance EPS at the same concentration and immersion temperature as the Steris System 1—is not responsible for the endoscope damage associated with the System 1.
An evaluation of the Steris Reliance EPS features a manufacturer’s claim that peracetic acid is not the cause of endoscope damage associated with the Steris System 1. The medical literature was reviewed to evaluate whether this claim is evidence-based. The results of this review are discussed herein.
Rather, Steris contends in ECRI’s evaluation that peracetic acid uncovers “prior defects that had resulted from wear and tear and/or improper care and handling” of endoscopes by staff members, adding that these defects had been “masked by aldehyde-based” disinfectants, such as 2% glutaraldehyde and ortho-phthalaldehyde, previously used to reprocess these endoscopes.
Click here to read Dr. Muscarella’s article, entitled “Review of an Evaluation of the STERIS Reliance EPS Reprocessor,” which reviews ECRI’s evaluation of the Steris Reliance EPS.
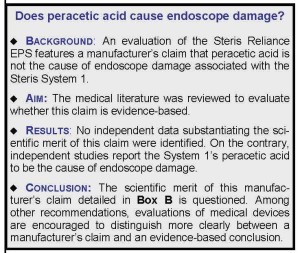
The medical literature was reviewed to evaluate the validity of this manufacturer’s claim and explanation of the cause of endoscope damage associated with the System 1. The results of this review raise questions about the scientific merit of this claim. No independent studies or data were identified that substantiate this manufacturer’s claim. Rather, this review identified published studies that report the System 1’s peracetic acid to be the cause of damage to endoscopes.
BACKGROUND
Another article (click here to read it) features Dr. Muscarella’s review of an evaluation of the Steris Reliance Endoscope Processing System (“EPS”)—a recently introduced automated endoscope reprocessor (“AER”) labeled to wash and high-level disinfect gastrointestinal (GI) endoscopes.(1) Authored by the ECRI Institute (“ECRI”), this evaluation rates the Reliance EPS “preferred over traditional AERs for facilities that use compatible endoscopes.”(2)
Further, ECRI’s evaluation “strongly encourage(s) healthcare facilities … that do not have Pentax endoscopes … to purchase the Reliance EPS rather than a traditional AER.”(2)
To be sure, this commendatory rating and firm instruction would be salient and warrant attention if it were evidence-based. Yet, while this evaluation provides some important details about the Reliance EPS, such as this AER’s use of a pressurized “boot,”(2) this rating and instruction are difficult to rationalize and justify.
Discussed in Dr. Muscarella’s article that reviews ECRI’s evaluation of the Steris Reliance EPS, two oversights are identified that raise legitimate questions about the quality and scientific merit of the rating and instruction of this evaluation by ECRI.(1,2)
First, this evaluation did not conduct any performance or microbiologic tests as would be required to rate the effectiveness and safety of the Reliance EPS.(1,2) Second, this evaluation did not include or test any of these disfavored “traditional” AERs to which the Reliance EPS was compared.(1,2) (A review of both this article #1 and this other article #2 is necessary to place this article herein about endoscope damage in the proper context.)
ECRI rates a product preferred if it “meets all major performance and safety criteria … and offers significant advantages over other alternatives.”(2)
Which raises a fair question: What was the scientific rationale for rating the Reliance EPS “preferred,” realizing that this evaluation did not conduct any performance or safety tests and did not include for comparison any of these “alternative” AERs?
Whether interactions with manufacturers might have played a role in rating this AER, compromised this evaluation’s quality, or contributed to its incompleteness is also a fair question to ask.(1)
Click here to read Dr. Muscarella’s blog entitled “Let Sleeping Dogs Lie? The Importance of Disclosure in Infection Control,” which discusses the potential for biases to affect “working relationships” between manufacturers and, for example, organizations that rate a medical device’s effectiveness.
A MANUFACTURER’S CLAIM?
Also discussed in this article, ECRI’s evaluation of the Reliance EPS does not, at times, clearly distinguish a manufacturer’s promotional (and unsubstantiated) claims from evidence-based conclusions—another of this evaluation’s more significant oversights.(1,2)
For example, ECRI’s evaluation concludes that the Reliance EPS “eliminates” personnel exposure to peracetic acid and its fumes, and that this AER “disinfects (the GI endoscope’s) suction valves.”(1,2) But, ECRI’s evaluation did not perform the necessary air sampling and microbiologic tests, respectively, to render these two conclusions—suggesting that each is a manufacturer’s claim, not an evidence-based conclusion.
As if in a tone of exoneration, ECRI’s evaluation of the Steris Reliance EPS recites and advances a manufacturer’s account of the cause of endoscope damage acknowledged to be associated with the Steris System 1.(1-3,7)
Nevertheless, no example might be more evident of the failure to distinguish clearly a manufacturer’s claim from an evidence-based conclusion than this evaluation’s discussion of materials’ incompatibility and the cause of endoscope damage associated with the Steris System 1.
The importance of distinguishing a manufacturer’s claim from an evidence-based finding cannot be overstated.
ENDOSCOPE DAMAGE
Although ECRI’s evaluation of the Reliance EPS does not rate the performance of the Steris System 1 (both models are marketed by Steris and flush the flexible endoscope’s internal channels under pressure with peracetic acid at an elevated temperature, although the System 1 claims to achieve “sterilization”), this evaluation nevertheless acknowledges the System 1’s association with endoscope damage.(2)
Because the Reliance EPS uses peracetic acid at the same concentration and elevated immersion temperature as the System 1 (the immersion times of the two processes are slightly different),(3) ECRI’s evaluation concedes that the Reliance EPS, too, may be associated with endoscope damage.(2)
As if to clarify an ongoing misunderstanding about peracetic acid, ECRI’s evaluation recites—without a rebuttal or a debate of its scientific merit—a manufacturer’s controversial three-part claim to explain the Steris System 1’s association with endoscope damage.(2)
Provided in Box B (there is no ‘Box A‘ included in this article), this manufacturer claims that peracetic acid uncovers “prior (endoscope) defects that had resulted from wear and tear and/or improper care and handling” by staff.(2)
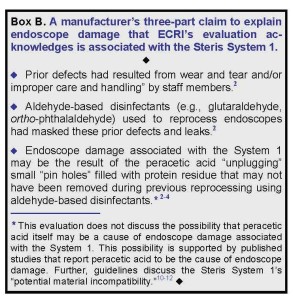
This manufacturer adds in ECRI’s evaluation that: (i) these defects and endoscope leaks had been “masked” by aldehyde-based disinfectants, such as 2% glutaraldehyde and 0.55% ortho-phthalaldehyde (e.g., Metricide and Cidex OPA, respectively); and that: (ii) the damage associated with the System 1 “may be the result of the peracetic acid removing protein residue” that was not removed by these aldehyde-based disinfectants (see: Box B) used previously to reprocess these endoscopes.(2-4)
Noteworthy, however, ECRI’s evaluation of the Reliance EPS does not present any corroborating data or cite any independent studies to substantiate this three-part claim—which is advanced in this evaluation and also in some of this manufacturer’s advertisements.(2-4)
Nor does this evaluation provide any other plausible or alternative account (save this manufacturer’s) to explain the cause of endoscope damage associated with the System 1. The possibility that peracetic acid itself might be responsible is ignored in this evaluation.
Whether this manufacturer’s claim is scientifically sound or lacks merit warrants examination.
(Note: The sale of the Steris System 1, which the FDA declared in May 2008 has been “adulterated and misbranded” since 1988, was discontinued in January 2009.[5,6] Click here to read Dr. Muscarella’s blog that discusses this product’s history, discontinuation and de facto recall.)
AIM AND METHODOLOGY
The medical literature, published infection-control guidelines, and the operator’s manuals of a few flexible and rigid endoscopes were reviewed to investigate the scientific merit of this manufacturer’s claim that, not peracetic acid, but rather wear, tear, and/or improper care and mishandling of endoscopes by staff, “masked” by aldehyde-based disinfectants used previously during reprocessing, are the causes of the endoscope damage associated with the Steris System 1 (and, possibly, with the Reliance EPS).
Click here to read Dr. Muscarella’s blog that reviews an institute’s evaluation of the performance of the Steris Reliance EPS.)
RESULTS
No independent studies were identified during this review that scientifically substantiate this manufacturer’s account and demonstrate that peracetic acid is not the cause of endoscope damage associated with the Steris System 1.
Nor did this review identify any independent reports that suggest endoscopes reprocessed using an aldehyde-based disinfectant, whether or not subsequently reprocessed using peracetic acid, are more prone to damage and leaks than the same models of endoscopes (e.g., identically worn, aged, cared for and handled) reprocessed exclusively using the System 1.
No independent data substantiating the scientific merit of this claim were identified. On the contrary, independent studies report the System 1’s peracetic acid to be the cause of endoscope damage.
On the contrary, this review identified two independent, peer-reviewed studies that identify the Steris System 1 as the cause of endoscope damage,(7,8) this manufacturer’s claim advanced in ECRI’s evaluation notwithstanding. Both of these two studies used methodologies that ruled out either aldehyde-based disinfectants or routine wear, tear, and/or improper care and mishandling of endoscopes as possible causes of endoscope damage. The first of these two studies published in 1997 was not discussed or cited in ECRI’s evaluation,(7) and no erratum published by ECRI discussing either of these studies was identified during this review.
Two other articles suggest that peracetic acid may “unplug” small “pin holes” inside the endoscope that become filled with patient debris not removed during previous reprocessing using aldehyde-based disinfectants (see: Box B).(2-4) Both suggest that, by removing this “protein residue,” the Steris System 1’s peracetic acid uncovers (but is not the cause of) endoscope damage.(2-4) Neither article was peer-reviewed, however, and, providing claims similar to those in ECRI’s evaluation, both were sponsored and authored by Steris.(3,4,9)
Further, this review identified published guidelines stating that 2% glutaraldehyde and ortho-phthalaldehyde display “excellent material compatibility” but that the System 1’s peracetic acid is associated with “potential material incompatibility.”(10-12)
One manufacturer (Olympus America) has raised concerns about the potential for the Steris System 1 to cause “chemically induced damage” to its GI endoscopes.(13) Another manufacturer (Pentax) lists the System 1’s peracetic acid as an agent that is “compatible” with its GI endoscopes,(14) but this same manufacturer contraindicates the use of the Reliance EPS for reprocessing any of its endoscopes.(2) A manufacturer of rigid and flexible endoscopes (Karl Storz) states that the System 1 can be used to reprocess its endoscopes.(15,16)
No independent data were identified during this review that substantiate the validity of the claim that, not peracetic acid, but masked defects, improper care or mishandling by staff, plugged holes, or aldehyde-based disinfectants are the causes of endoscope damage associated with the System 1.(2)
DISCUSSION
The scientific soundness of this manufacturer’s three-part claim, which is provided in Box B which ECRI advances in its evaluation of the Reliance EPS, to explain the cause of endoscope damage associated with the Steris System 1 is questioned.
Similarly questioned is the balance, validity, and completeness of ECRI’s evaluation of the Reliance EPS, primarily for having failed to have: performed any safety, effectiveness, or materials’ compatibility tests; included and tested any of the disfavored “traditional” AER models; and distinguished more clearly between a manufacturer’s claim and an evidence-based result. (Click here to review Dr. Muscarella’s article about the Steris Reliance EPS.)
This article questions the scientific merit of this manufacturer’s claim detailed in Box B, above. Among other recommendations, evaluations of medical devices by organizations including the ECRI Institute are encouraged to distinguish more clearly between a manufacturer’s claim and an evidence-based conclusion. Additional recommendations are provided in the second article in this series: “Endoscope Damage Part 2.”
In general, a study’s inclusion and discussion of a manufacturer’s controversial claim, without providing an accompanying rebuttal or questioning the claim’s merit for perspective and soundness, might be justifiable, provided that certain criteria are met—for example, that independent studies have verified the claim’s plausibility, if not merit; or, certainly, that no independent studies refuting this claim’s soundness have been published. Otherwise, the inclusion, if advancement, of this manufacturer’s claim might cause the study to appear partial, incomplete, or concessionary.(1)
But such criteria most certainly were not met, and ECRI’s evaluation of the Reliance EPS did not provide or cite any independent data to substantiate the scientific merit of this manufacturer’s three-part claim.(2) To the contrary, scientific studies report that the Steris System 1’s peracetic acid—not protein residue, masked defects, or aldehyde-based disinfectants —caused damage to endoscopes, some of which were brand new.(7,8)
That ECRI’s evaluation acquiesces, presumes its a priori legitimacy and soundness, and neither debates, rebuts, nor questions the validity of this manufacturer’s claim is difficult to understand. Perhaps even more confusing is ECRI’s failure to provide, as seemingly necessary for balance, an alternative explanation—for example, to raise for discussion the manifest possibility that peracetic acid itself might be (at least in part) responsible for the System 1’s noted association with endoscope damage.(2)
Indeed, ECRI’s evaluation of the Reliance EPS attributes this expressed three-part claim of the cause of endoscope damage to the manufacturer (see: Box B). But, its evaluation’s concurrent failure to investigate and probe this claim’s validity; to note that this manufacturer’s claim has not been independently substantiated; and—most important—to cite and discuss scientific studies that contrarily report peracetic acid to be the cause of the endoscope damage associated with the System 1(7,8) causes, at best, unnecessary confusion.
Blurring the line that distinguishes a manufacturer’s claim from an evidence-based finding, these oversights raise important questions about the objectivity of ECRI’s evaluation and of its discussion of the causes of endoscope damage.
This article’s references are available here.
Article by: Lawrence F Muscarella PhD; updated 5-15-2014, Rev A.